Proudly Part of Privia Health
Arthritis/Cartilage Replacement
What Is Osteoarthritis?
Osteoarthritis is a condition characterized by the breakdown and eventual loss of cartilage in one or more joints. Cartilage (the connective tissue found at the end of the bones in the joints) protects and cushions the bones during movement. When cartilage deteriorates or is lost, symptoms develop that can restrict one’s ability to easily perform daily activities.

Osteoarthritis of the great toe joint, note loss of cartilage and marginal bone spurs
Osteoarthritis is also known as degenerative arthritis, reflecting its nature to develop as part of the aging process. Osteoarthritis appears at various joints throughout the body, including the feet and ankles. In the foot, the disease most frequently occurs in the big toe, although it is also often found in the 2nd MTPJ, the midfoot and the ankle.
Causes
Osteoarthritis is considered a wear-and-tear disease because the cartilage in the joint wears down with repeated stress and use over time. As the cartilage deteriorates and gets thinner, the bones lose their protective covering. Eventually the two bones rub together and cause pain and inflammation of the joint.
An injury may also lead to osteoarthritis known as traumatic arthritis. This may take months or years after the injury to develop. For example, osteoarthritis in the big toe may be caused by kicking or jamming the toe during sports. Osteoarthritis in the midfoot may be caused by dropping something on it or by a sprain or fracture (“Lisfranc” fracture-dislocation). In the ankle, the most common causes of cartilage are acute or chronic injuries such ankle sprains, dislocations, fractures, or instability.
Sometimes osteoarthritis develops as a result of abnormal foot mechanics, such as flat feet or high arches. A flat foot causes less stability in the ligaments (bands of tissue that connect bones), resulting in excessive strain on the joints leading to arthritis. A high arch is rigid and lacks mobility, causing a jamming of joints that creates an increased risk of arthritis.
Symptoms of Osteoarthritis/Cartilage Damage
People with cartilage damage or osteoarthritis in the foot or ankle experience, in varying degrees, one or more of the following:
- Pain and stiffness in the joint
- Swelling in or near the joint
- Dull or aching pain deep within the joint
- Inflammation
- Weakness
- Limited mobility
- Locking or catching feeling
- Difficulty walking or bending the joint
Some patients also develop a bone spur (a bony protrusion) at the affected joint or a loose body or piece of articular cartilage. Shoe pressure may cause pain at the site of a bone spur, and in some cases, blisters or calluses may form over its surface. Bone spurs can also limit the movement of the joint.
Diagnosis
In diagnosing osteoarthritis and cartilage injuries, the foot and ankle surgeon will examine the foot thoroughly, looking for swelling in the joint, limited mobility and pain with movement. In some cases, deformity and/or enlargement (spur) of the joint may be noted. X-rays may be ordered to evaluate the extent of the disease. Typically, a weight-bearing (standing) x-ray is ordered to view the foot and ankle bone anatomy. An x-ray will show if there is substantial arthritis or damage that goes deep into the bone. However, sublets cases will require an MRI for a more detailed view of the joint to determine if there are any osteochondral injuries or defects present.
MRIs are most commonly indicated among younger patients or athletes with recalcitrant pain or swelling in the joint that has not responded to conservative care using RICE (rest, ice, compression, elevation) and immobilization.
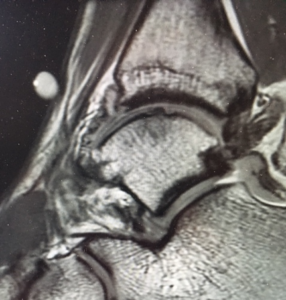
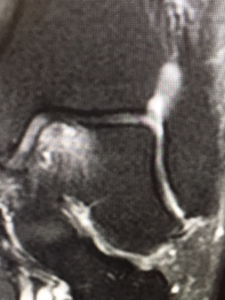
Osteochondral (bone/cartilage) defect on MRI
Conservative/Nonsurgical Treatment
Treatment options vary depending on the extent of the osteoarthritis and if a cartilage injury is present. Additionally, patient factors such as age, weight, health and performance level need to be taken in to account.
To help relieve symptoms, the surgeon may begin treating cartilage injuries and osteoarthritis with one or more of the following nonsurgical approaches:
Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), are often helpful in reducing the inflammation and pain.
Orthotic devices. Custom-molded orthotic devices (shoe inserts) are often fabricated to provide support to improve the foot’s mechanics or cushioning to help minimize pain.
Bracing. Bracing, which restricts motion and supports the joint, can reduce pain during walking and can help prevent further deformity.
Immobilization. Protecting the foot from movement by wearing a cast or removable cast-boot may be necessary to allow the inflammation to resolve.
Steroid injections. In some cases, steroid injections are applied to the affected joint to deliver anti-inflammatory medication.
Physical therapy. Exercises to strengthen the muscles, especially when osteoarthritis occurs in the ankle, may give the patient greater stability and avoid injury that might worsen the condition.
Intra-articular injections, such as platelet-rich-plasma, may be considered as a short-term option to reduce inflammation, ease pain, and promote healing if a cartilage injury is present.
Surgical Treatment
When conservative treatment is unsuccessful or a cartilage lesion has progressed beyond the point of healing, surgical intervention may be necessary to repair the damage. Additionally, any predisposing factors such as foot deformity or joint laxity must be addressed to prevent recurrence and protect and offload the repair. The goal of surgery is to decrease pain and improve function. The foot and ankle surgeon will consider a number of factors when selecting the procedure best suited to the patient’s condition and lifestyle.
Ankle Arthroscopy
Arthroscopic surgery on the foot and ankle may be used as a diagnostic or treatment procedure, or both. A small instrument, called an arthroscope, penetrates the skin through small incisions. Tiny cameras can be inserted through the arthroscope, allowing the surgeon to accurately see the area and/or damage. Other small instruments can also be inserted through the arthroscope to make surgical corrections.
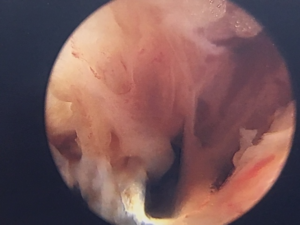
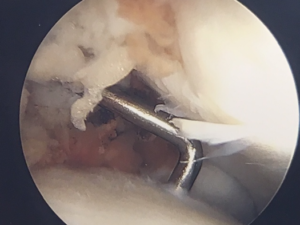
Ankle synovitis (joint lining) arthroscopic removal for chronic inflammation
Partial joint lining removal, completed

Ankle arthroscopy, assessing cartilage

Posterior ankle scope, small incisions healing well
Because arthroscopy is less invasive and traumatic than traditional surgery, it reduces the risk of infection and swelling and allows for significantly speedier healing and recovery. Most arthroscopic surgeries of the foot and ankle are performed on a same-day, outpatient basis using a local anesthetic.
Ankle injuries can cause damage to the smooth cartilage surfaces in the joint, whether from a simple sprain or a fractured bone. The most common cartilage injury is an osteochondral defect (OCD) of the talus (the floor) or the tibia (ceiling of the joint). Talar dome lesions are usually caused by an injury, such as an ankle sprain. If the cartilage does not heal properly following the injury, it softens and begins to break off. Sometimes a broken piece of the damaged cartilage and bone will float in the ankle. The signs and symptoms include chronic pain deep in the ankle that are typically worse when bearing weight on the foot, especially during sports and less when resting; an occasional clicking or catching feeling in the ankle when walking; a sensation of the ankle locking or giving out; and episodes of swelling of the ankle that occur when bearing weight and subsiding when at rest. The goal of surgery is to remove the loose or damaged cartilage from the ankle and replace it with a healthier cartilage surface to restore a smooth surface for proper, pain-free gliding of the joint.
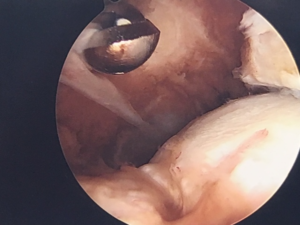
Ankle scope, finding cartilage defect
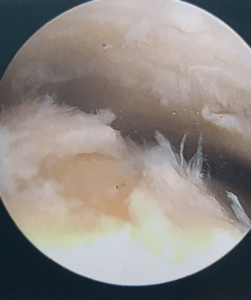
Ankle scope, cleaning up cartilage defect
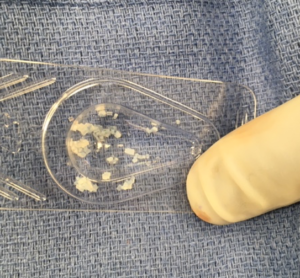
Juvenile cartilage graft material for cartilage defect, ankle
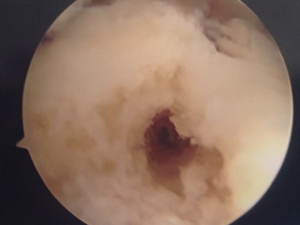
Microfracture, talus (ankle) for growth of fibrocartilage

Arthroscopic spur removal, ankle, with power burr
Microfracture/Bone Marrow Stimulation
The simplest type of cartilage repair small simple cartilage injuries is called microfracture or bone marrow stimulation. This outpatient surgery is performed with minimally invasive arthroscopy using small cameras and arthroscopic instruments. This microfracture technique is used to promote cartilage development thereby facilitating healing.
Through an arthroscopic surgery, inflammation called synovitis, fragments and debris are removed or “cleaned out” and loose or damaged sections of bone and tissue are removed to create a stable crater. Tiny holes are then created with a small tool that resembles a pick or awl into the bone’s surface. This releases a combination of blood and bone marrow from below to form a blood clot that covers the bone and fills the crater, and over the next several months will stimulate the development of fibrocartilage.
In smaller osteochondral injuries, this type of repair can give excellent results allowing patients to return to their pre injury activities including running and sports.
Juvenile Allograft Transplantation
Juvenile allograft transplantation, sometimes known as the DeNovo natural tissue graft implantation, performed to replace damaged cartilage in the ankle with cartilage from a donor. DeNovo Natural Tissue Graft is an alternative to other cartilage treatment options in the ankle, where it is often used as a primary treatment option for lesions larger than one square centimeter or as a secondary treatment option to previous cartilage repair treatments that have failed. Juvenile allograft transplantation received its name because the healthy cartilage tissue used for the procedure is harvested from donors under the age of 13.
The DeNovo Natural Tissue Graft is an off-the-shelf human tissue allograft contains juvenile hyaline cartilage pieces with viable chondrocytes, and is intended for the repair of articular cartilage lesions in a single-stage procedure. Since juvenile tissue contains a greater quantity of chondrocytes, or healthy cartilage cells, than adult tissue (10x greater) it provides patients a greater chance of the joint healing.
Juvenile allograft transplantation is performed as a minimally invasive technique in conjunction with ankle joint arthroscopy. The surgery is performed under twilight anesthesia in a same day surgery. It is an alternative to more intrusive cartilage treatments since it eliminates the need to harvest tissue from areas of undamaged cartilage and avoids ankle osteotomies (surgically created fractures). At times the procedure may be combined with a subchondroplasty. The Subchondroplasty® Procedure is a minimally-invasive, fluoroscopically-assisted procedure that targets and fills subchondral bone defects, sometimes called Bone Marrow Lesions that maty be associated with cartilage lesions. It is usually performed along with arthroscopy, for visualization and treatment of findings inside the joint. The lesion is filled with AccuFill® Injectable Bone Substitute Material, which is a bone graft substitute that resorbs and is replaced with new bone during the healing process. Finally, any preoperatively-noted ligament laxity is surgically addressed at the time of the DeNovo grafting to ensure a stable and naturally functioning ankle joint. Overall, the main goal of this procedure is to relieve pain and restore normal movement and function to the ankle.
Osteochondral Graft/OATS/Moasicplasty
For larger cartilage injuries or in certain situations where the anatomy prevents juvenile cartilage application there is another surgical option. The OATS procedure, osteoarticular transfer system , or mosaicplasty may be performed. This is an operation for is for isolated cartilage defects of the ankle (talus or tibia).. The surgery uses healthy cartilage from undamaged areas of the knee to replace the injured areas of the ankle. A cylinder of bone and overlying cartilage from the patient’s own knee, or from a cadaver, is placed into the into the ankle joint cartilage defect that has been already cored out to restore a smooth surface. This is an open procedure and access to the ankle joint defect is usually achieved by cutting (osteotomy) one of the bones of the ankle (medial or lateral malleolus), to expose the cartilage lesion. At the end of the grafting procedure the ankle fracture is repaired as well.
ProChondrix CR Cryopreserved Fresh Osteochondral Allograft
Cartilage defects and injuries in smaller joints have fewer option due to the location and anatomy of the joints. For smaller lesion like, in the ankle, microfracture still remains a viable option. However, for larger lesion the options become more limited due to the very thin nature of the involved cartilage. For these joints a ProChondrix Osteochondral graft can be performed, such as in the 2nd metatarsal phalangeal joint. This joint often sustains larger osteochondral defect that require surgical repair.
ProChondrix CR is a cryopreserved, fresh osteochondral allograft that contains live cells and other biological components for the repair of damaged cartilage tissues. Prochondirx CR can be used in a variety of reconstructive procedures to aid in the repair of articular cartilage. This graft is designed to help support a structure for cellular migration and adhesion while preserving growth factors thereby maintaining healthy cartilage and facilitate chondrocyte functionality. These viable chondrocytes have been shown to be present and may aid in cartilage repair promote chondrogenesis, or the growth of new cartilage.
Cartilage defect removal

Cartilage defect, repaired with cartilage graft

Platelet Rich Plasma Treatment
Platelet-rich plasma, PRP injections, are a treatment method that uses components of the body’s own blood to stimulate healing. Platelets are known for their role on clotting blood. They also contain hundreds of proteins called growth factors. These growth factors, according to recent research, are able to assist in the healing and strengthening of damaged tissues. PRP is plasma with 5 to 10 times greater than usual concentration of these platelet derived growth factors thereby activating, promoting and accelerating the healing process.
Conditions Treated with PRP Injections
Platelet-rich plasma injections can be used to treat a wide range of orthopedic conditions, including:
- Arthritis
- Chronic Tendonitis
- Acute Ligament sprains or tears
- Postsurgical healing from tendon or ligament repair
The PRP Procedure
The procedure is performed in our office. To develop a PRP preparation, blood is drawn from the patient. The blood is then spun down in a centrifuge to separate and concentrate the platelets from other blood cells. This platelet-rich concentrate is then injected into the area of injury with the assistance of ultrasound imaging. At times the area may be anesthetized prior to the injection with a local anesthetic. Most patients experience little or no discomfort from the injection. There may be some post-injection soreness of inflammation for 24- 48 hours. Depending on the location and injury being treated a period of immobilization may be required.
Benefits of PRP Injections
Benefits of the procedure can take up to 6 weeks to occur. There are several benefits to using PRP therapy. These include the fact that the platelet-rich plasma being injected is autologous (comes from the patient). PRP injections are very minimally invasive. Finally, PRP injections facilitate healing in both acute and chronic injuries.
Bone Marrow Aspirate
Bone marrow aspirate concentrate (BMAC) is made from fluid taken from the patient’s own bone marrow. The aspirate is placed into a centrifuge producing a biologic product that is rich in stem cells and growth factors. The bone marrow is typically harvested through the tibia or calcaneus (heel bone). The BMAC can then be injected during a surgical procedure in the foot or ankle to increase and promote healing. BMAC or stem cells can be used to help with bone and cartilage healing. Typically, BMAC is used to treat delayed union or non-unions of fractures, cartilage defects/injuries, difficult fusions, chronic tendon problems, or chronic wounds. Typically the harvest site pain, if presents, resolves in 5-7 days.