Surgery on the foot, ankle or lower leg is usually performed by podiatric surgeons and orthopedic surgeons specializing in the foot and ankle.
Foot and ankle surgeries address a wide variety of foot problems, including:
- Sprains and fractures.
- Arthritis and joint disease.
- Benign and malignant tumors.
- Birth deformities.
- Bunions.
- Calluses and warts.
- Corns and hammertoes.
- Flatfeet.
- Heel or toe spurs.
- Neuromas (nerve tumors).
Many foot and ankle surgeries today can be performed in the doctor’s office or a surgical center on an outpatient basis. They frequently can be performed using local anesthesia, in some cases combined with sedation. Most foot surgeries require a period of immobilization after the procedures with protective devices, such as bandages, splints, surgical shoes, casts, or open sandals. Limited weight bearing, elevating and icing the foot, and keeping the area dry are commonly required for the first two weeks following surgery until sutures are removed. Most surgeons will encourage post-operative exercise of the foot and legs to speed recovery. In addition, many patients need additional therapy or treatments after surgery in order to aid in the healing and recovery process. These may include physiotherapy, orthotic devices, and special footwear. After sufficient healing time, which varies from procedure to procedure, most patients can resume wearing their usual footwear.
Surgery to repair a torn (ruptured) Achilles tendon is conducted on an outpatient basis using a local anesthetic. It involves making an incision or cut in the back of the leg above the heel to access the torn tendon. The tendon is then sewn back together. Surgery may be delayed for about one week after the rupture to let the swelling go down.
After surgery, a cast or walking boot is usually worn for six to 12 weeks. At first, the cast or boot is positioned to keep the foot pointed downward as the tendon heals. The cast or boot is then adjusted gradually to put the foot in a neutral position (not pointing up or down).
Specific gentle exercises (restricted motion) after surgery can shorten the time needed for rehabilitation.
Patients who undergo surgery to correct arthritis in the foot are often diabetics with a type of arthritis known as Charcot Foot. The average age of patients developing a Charcot foot is 40 years. About one-third of patients develop a Charcot foot in both feet and/or ankles. This form of arthritis can develop suddenly and without pain. Quite suddenly, the bones in the foot and/or ankle can spontaneously fracture and fragment, often causing a severe deformity.
The arch of the foot often collapses, and pressure areas develop on the bottom of the foot, leading to open sores or ulcers.
While many of these deformities can be treated with nonsurgical care, surgery may be required. Such instances may include:
- Chronic deformity with increased plantar pressures and risk of ulcers.
- Chronic deformity with significant instability that cannot be corrected by braces.
- Significant deformity that may include ulcers that don’t heal or respond to therapy.

Surgical procedures used to treat arthritis include:
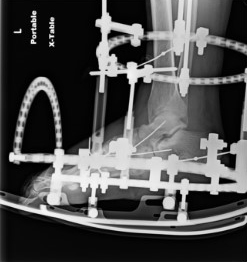
- Hindfoot and ankle realignment. This kind of procedure is usually prescribed when there is significant instability resulting in a patient being unable to walk. Various types of internal fixation are placed within the foot during this kind of procedures.
- Midfoot realignment. This kind of procedure is usually prescribed when there is significant instability of the middle portion of the foot. During a midfoot realignment, various types of internal fixation are placed within the foot.
- Ostectomy. In this procedure, a portion of bone is removed from the bottom of the foot. It is usually performed for a wound on the bottom of the foot that is secondary to pressure from a bony prominence.



Ganglion masses, or cysts, are normally removed through surgery. Most cyst removal surgeries are performed on an outpatient basis. Contact our office to have this procedure performed.
During the procedure, the cyst is dissected from the surrounding soft tissues and removed. The recovery period depends on the location of the ganglion and the amount of dissection required during surgery. In many cases, patients receive a splint or below-the-knee cast. The surgeon may require the patient to use crutches for several days to up to three weeks. This level of protection may be necessary if the ganglion is near the ankle joint.
Possible complications from cyst removal surgery include infection, excessive swelling, and nerve damage.
Many conditions can affect the rear part of the foot and ankle. Two common conditions can cause pain to the bottom of the heel and lead to surgical intervention: plantar fasciitis (an inflammation of a fibrous band of tissue in the bottom of the foot that extends from the heel bone to the toes) and heel spurs (often the result of stress on the muscles and fascia of the foot).
There are many causes of heel pain and most cases can be effectively treated without surgery. Chronic heel pain, however, often can be corrected only through surgery.
A surgical procedure, called an osteotomy, is performed to relieve the pressure on the bone from heel calluses. The procedure involves cutting the metatarsal bone in a “V” shape, lifting the bone and aligning it with the other bones. This alleviates the pressure and prevents the formation of a heel callus.
A neuroma is an abnormality of a nerve that has been damaged either by trauma or as a result of an abnormality of the foot. Neuromas occur most often in the ball of the foot, causing a pinched and inflamed nerve. In cases of chronic nerve pain from neuromas, surgery may be recommended.
During neuroma procedures, an incision is made on the top of the foot in the location of the neuroma, usually between the second and third toes or between the third and fourth toes. After the nerve is located, the surgeon cuts and removes it.
Neuroma surgery is generally performed on a same-day outpatient basis in the doctor’s office or a surgery center using a local anesthetic. The incision will be covered with a dressing after the surgery, which must be kept dry until the sutures are removed, usually within 10 to 14 days after the surgery. Most patients are sent home with a surgical shoe, although crutches may be recommended in cases where the incision must be made on the bottom of the foot. Elevation and icing are important in the first few days following surgery to reduce swelling. Patients are generally restricted to limited walking until the sutures are removed. Generally, patients can return to normal shoe wear in about three weeks. The overall recovery time is usually four to six weeks.